Enhanced Recovery After Surgery
Enhanced Recovery After Surgery Overview
Enhanced Recovery After Surgery (ERAS®) refers to patient-centered, evidence-based, multidisciplinary team developed pathways for a surgical specialty and facility culture to reduce the patient’s surgical stress response, optimize their physiologic function, and facilitate recovery.
These care pathways form an integrated continuum, as the patient moves from home through the pre-hospital / preadmission, preoperative, intraoperative, and postoperative phases of surgery and home again.
The AANA provides a wealth of resources for Enhanced Recovery After Surgery, including:
- Practice considerations
- Protocols
- ERAS program elements
- Implementation
- ERAS roles
Enhanced Recovery at a Glance Infographic Series
ERAS: Pre Hospital
ERAS: Pre Operative
ERAS: Intra Operative
ERAS: Post Operative
ERAS: Post Discharge
ERAS: Audit Compliance
Elements of an ERAS program
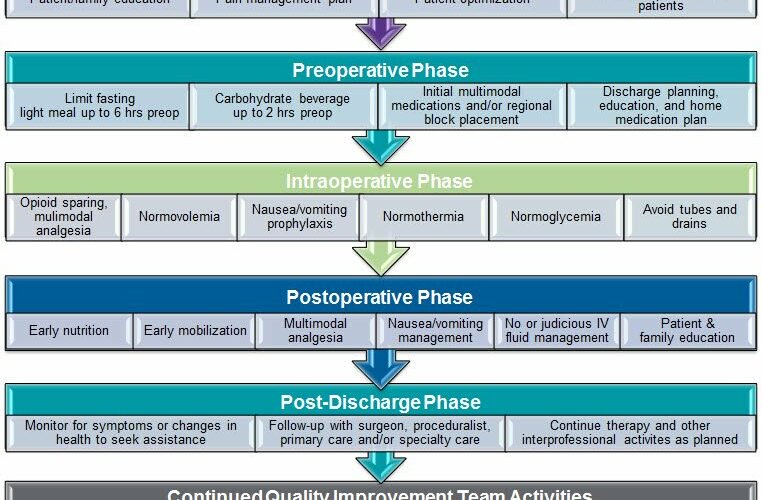
Though individual elements of an ERAS pathway are beneficial, implementation and compliance with patient appropriate elements of a comprehensive pathway across the entire perioperative continuum have been shown to improve outcomes. The key elements of ERAS include patient/family education, patient optimization prior to admission, minimal fasting that includes a carbohydrate beverage two hours before anesthesia, multimodal analgesia with appropriate use of opioids when indicated, return to normal diet and activities the day of surgery, and return home.
ERAS Program Phase Chart
ERAS Program Phase Chart
Anesthesia professionals deliver many of the enhanced recovery elements that are summarized in the figure below.
Advantages of Implementation
Advantages of Implementation
Research has consistently shown that adoption of enhanced recovery leads to significant improvements in patient satisfaction, outcomes and reduction in cost of care. Specifically, patients experience faster recovery, shortened hospital stay and significantly fewer complications. To successfully integrate ER into practice, a structured, collaborative, multidisciplinary approach accompanied by education and awareness campaign may be valuable.
Implementation
Implementation
Successful change management and ERAS implementation occurs as a process that evolves from leadership, creation of the climate for change, and engagement and empowerment of those involved, through the development of a change initiative, implementation or trial of the pathway, and sustained change with continued improvement.
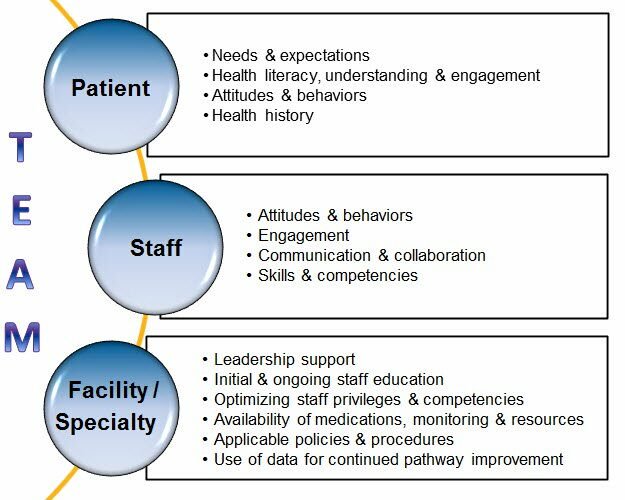
Specific areas where ERAS programs have faced implementation challenges may be attributed to the following:
- patient-related;
- staff-related; and
- practice-related factors.
Recognition of these challenges in the development and improvement of your program may be helpful for the long-term success of an ERAS program.
The Role of the ERAS Coordinator
The Role of the ERAS Coordinator
This article is by Kelsey Terrones, CRNP, ERAS Coordinator, Greater Baltimore Medical Center.
As most clinicians and health organizations can attest, incorporating and implementing new evidence-based practice changes almost always involves overcoming some challenges and obstacles on the road to success. Common obstacles are often provider and upper management endorsement as well as financial resource and time allocation. Here, I will examine the effect of these obstacles on the creation of the Enhanced Recovery After Surgery (ERAS) Coordinator role at Greater Baltimore Medical Center (GBMC).
In August of 2016, Kara Douglas, CRNA alongside Dr. John Kuchar created and implemented the ERAS program, initially for the colorectal service line, at GBMC. In September 2016, I returned to GBMC as a nurse practitioner in GBMC’s Pre-Surgical Testing Center (PTC). My role included pre-operative patient care coordination and diagnostic testing. In June 2017, I was selected to join GBMC’S ERAS team as the ERAS Coordinator. This position created to help promote the success of our ERAS team led by Kara Douglas, MS, BSN, CRNA, ERAS Director, and Dr. Kuchar. This has been an incredibly challenging and rewarding opportunity as it is currently remains a dual-role position. The main challenge in this role is that I must balance my time between seeing patients for pre-operative evaluations as well as performing my duties as ERAS Coordinator.
Some of the ERAS Coordinator responsibilities I hold include: providing ERAS education for the patients pre-operatively, rounding on the hospital ERAS patients post-operatively, collecting and compiling patient data pertaining to our ERAS protocol adherence and evaluating patient outcomes. Lastly, Kara and I conduct at least one or two weekly meetings with key stakeholders from upper management, finance as well as our multidisciplinary team including EPIC analysts, physician/surgeon champions, nurse champions and nurse managers, physical and occupational therapies, dietitians/nutritionists and the Quality Department. This allows us to continue to advance our program and address problems as they arise.
When the patients come through the PTC for ERAS education, they receive an incentive spirometer, one or two bottles of Ensure Pre-Surgery (depending on the patient’s co-morbidities), a bottle of hibaclens (CHG) scrub and a folder of written instructions for these items as well as an overview of what to expect in the hospital and the purpose of the ERAS program. Unfortunately, it has been a challenge to see all of the patients undergoing ERAS procedures as not all choose to come through the PTC for the education session that lasts only 10-15 minutes and this is not mandatory education by the surgeons or GBMC.
ERAS in-patients are rounded on daily to collect key data points to evaluate compliance of our ERAS protocol as well as patient outcomes. Key data points include but are not limited to: patient ambulatory status, diet, time of return of bowel function, time of foley removal, pain evaluation and narcotic consumption.
Currently, GBMC is part of the improving surgical care and recovery (ISCR) but otherwise, does not utilize any formal system or platform for data collection/extraction and analysis. I am currently extracting all the various data points we are monitoring through individual chart audits in conjunction with patient rounding. This is a time consuming and labor-intensive data extraction and analysis process; however, we are examining various data capturing platforms from the ERAS societies to determine which would be the most beneficial platform for our institution. We have also been working closely with our EPIC team (our electronic medical record system) to develop audit features that can facilitate and expedite some of the information I am auditing from the individual charts.
GBMC’s ERAS program has been incredibly successful and has grown under the direction of Kara and support of Dr. Kuchar. This is largely due in part to their ability to network within and outside of our institution, as well as the work of our multidisciplinary team, endorsement and support from staff and upper management and personal and professional time investment. Many of the obstacles, namely time, resource allocation as well as coordination of the team, have been our hardest obstacles to overcome. For any institutional considering creating an ERAS program, based off our experiences with creating our ERAS program it is critical first and foremost that endorsement and support for your program is obtained from the institution’s key stakeholders and upper management. Lastly, proper time and role delineation should also be addressed and allotted as this will promote and ideally expedite proper expansion of the program to be instituted.
CRNA Contributions to ERAS Solutions
CRNA Contributions to ERAS Solutions
The following article by Carol Schmidt, MS, CRNA, Director, Anesthesia Services, Beaumont Hospital – Royal Oak, is presented by the Enhanced Recovery Shared Interest Group.
Enhanced recovery programs can range in complexity from highly complex to simple protocols designed to improve patient outcomes. The following is an example where Mary Beth Boeson, CRNA identified that patients age 65 years and older are at risk for postoperative delirium. After review of the literature she found that polypharmacy contributed to delirium. Working with the perioperative team she created a simple protocol for patients undergoing vitrectomy that eliminated medications that contribute to delirium and also reduced the amount of medication that was administered during the procedure. We used LMA over GET so we could avoid muscle relaxants and reversal agents. We engaged the patients and families to avoid the use of Versed.
Situation
Identified that patients age 65 or older are at risk for lengthy PACU stays and postoperative delirium. We found that this population sometimes received over 10 medications for the procedure.
Background
Evidence suggests that polypharmacy (the use of 5 or more medications) has been associated with increased risk of delirium. Additionally, the use of benzodiazepines, anticholinergics and antihistamines increase the risk.
Assessment
- Pre intervention
- 20 charts were audited (patients greater than 65 who underwent a vitrectomy under general anesthesia) to assess medication use and PACU length of stay
- 85 percent of patients received 2 mg Versed
- Average PACU length of stay was 100 minutes
- Post intervention
- 26 charts audited for the same population
- 53 percent decrease in the use of Versed
- 5 or less medications administered
- Average PACU length of stay was 73 minutes
Protocol
- Pre op
- Patient Engagement – Explain to the patient that you are going to avoid using sedative drugs that may linger delaying full recovery
- Intra op
- LMA
- Propofol/Etomidate
- Lidocaine 100mg IV
- Sevoflurane
- Zofran, if history of PONV
- Toradol 0.5 mg/kg IV
- LMA
- PACU
- Avoid IV opioid
Recommendations
Following a protocol that minimizes and/or eliminates polypharmacy reduces PACU length of stay by 30 minutes. We plan to assess for post op delirium in the future.
Additional Resources
ERAS Protocols, eBook, and Educational Resources
ERAS Protocols, eBook, and Educational Resources
Articles and White Papers
Articles and White Papers
- ERAS/STS 2024 Expert Consensus Statement on Perioperative Care in Cardiac Surgery: Continuing the Evolution of Optimized Patient Care and Recovery, Journal of Cardiothoracic and Vascular Anesthesia, October 2024
- The Future of Enhanced Recovery After Surgery—Precision vs Protocol, JAMA Open Network, June 2024
- Perioperative Care in Cardiac Surgery: A Joint Consensus Statement by the Enhanced Recovery After Surgery (ERAS) Cardiac Society, ERAS International Society, and The Society of Thoracic Surgeons (STS), The Annals of Thoracic Surgery, April 2024
- Enhanced Recovery After Surgery (ERAS) in Spine, Journal of Neurosurgical, April 2019
- Enhanced recovery after surgery: implementing a new standard of surgical care, CMAJ, April 2019
- Development and Implementation of a Colorectal ERAS Pathway, Clin Colon Rectal Surg, March 2019
- Guidelines for Perioperative Care in Gynecologic/Oncology: ERAS Update 2019
- Awake Lumbar Interbody Fusion
- American Society for Enhanced Recovery: Advancing Enhanced Recovery and Perioperative Medicine, Anesthesia & Analgesia, June 2018
- American Society for Enhanced Recovery and Perioperative Quality Initiative Joint Consensus Statement on Patient-Reported Outcomes in an Enhanced Recovery Pathway, Anesthesia & Analgesia, June 2018
- American Society for Enhanced Recovery and Perioperative Quality Initiative Joint Consensus Statement on Postoperative Gastrointestinal Dysfunction Within an Enhanced Recovery Pathway for Elective Colorectal Surgery, Anesthesia & Analgesia, June 2018
- American Society for Enhanced Recovery and Perioperative Quality Initiative Joint Consensus Statement on Nutrition Screening and Therapy Within a Surgical Enhanced Recovery Pathway, Anesthesia & Analgesia, June 2018
- Enhanced Recovery After Surgery: Implementation Strategies, AANA NewsBulletin, November 2017
- Development and Implementation of a Colorectal ERAS Pathway, Anesthesiology News, October 2017
- Perioperative Medicine – An open-access journal that publishes highly topical clinical research relating to the perioperative care of surgical patients.
- Why Cardiac Output?
- Physiology of Perfusion: Pressure and Flow
- Theory and Clinical Application of Continuous Fiberoptic Central Venous Oximetry (ScvO2) Monitoring
Disclaimer
The resources on this page may incorporate or summarize views, guidelines, or recommendations of third parties. Such material is assembled and presented in good faith, but does not necessarily reflect the views of the AANA. Links to third-party websites are inserted for informational purposes and do not constitute endorsement of the material on those sites, or of any associated organization.